Skin substitutes have emerged as a game-changing solution in wound care, offering hope to those dealing with chronic wounds, burns, and other skin injuries. Traditional wound healing methods, while effective to some extent, often come with limitations. The advent of skin substitutes is changing this landscape by providing alternative treatments that promote faster and more efficient healing. This article will delve into how skin substitutes work, their different types, and the impact they have on revolutionizing wound healing.
Understanding Skin Substitutes
Skin substitutes are engineered products designed to replace or aid the skin's natural healing process. Unlike conventional dressings, skin substitutes can act as a temporary or permanent solution, providing a protective covering, enhancing the wound environment, and promoting new tissue formation.
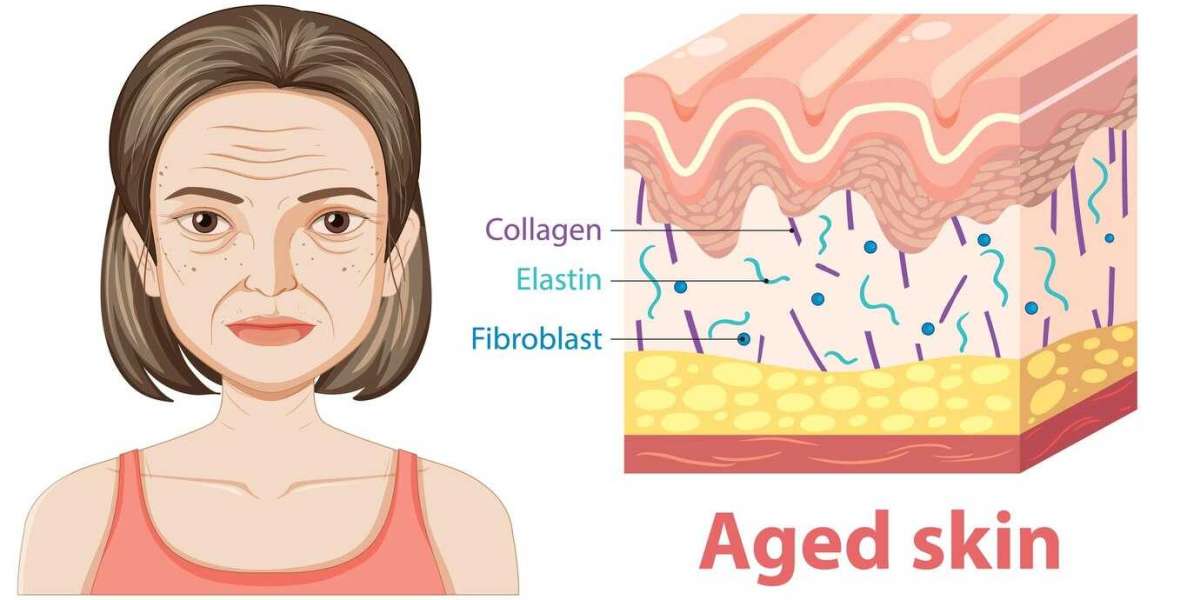
These substitutes mimic the skin’s structure, either partially or fully, to facilitate the body’s healing mechanisms. Depending on the wound's nature and severity, skin substitutes can be bioengineered using natural tissues, synthetic materials, or a combination of both. They create an ideal environment for wound healing by maintaining moisture, allowing oxygen to reach the wound, and preventing infection.
Types of Skin Substitutes
Several types of skin substitutes are available today, each serving different purposes depending on the wound type and treatment goals. They generally fall into three categories: biological, synthetic, and biosynthetic.
1. Biological Skin Substitutes
Biological skin substitutes are derived from natural human or animal tissues. These substitutes contain cells, growth factors, and proteins that are crucial for wound healing. Examples include:
- Allografts: Made from human donor skin, allografts act as a temporary cover to protect the wound and reduce fluid loss. They also provide a framework for new tissue growth.
- Xenografts: These come from animal sources, commonly pigs, and serve as a temporary wound covering that aids in moisture retention and healing.
- Cultured Epidermal Autografts (CEA): Created using a small sample of the patient's own skin cells, CEAs are grown in a lab to form new skin layers. This process is particularly beneficial for large burns or chronic wounds where skin availability is limited.
2. Synthetic Skin Substitutes
Synthetic skin substitutes are made from man-made materials like silicone, polyurethane, and other polymers. They provide a sterile environment for the wound, control fluid loss, and reduce the risk of infection. Synthetic substitutes are particularly useful when a long-term cover is required, and they can be designed to mimic the skin's natural properties.
3. Biosynthetic Skin Substitutes
These are a combination of biological and synthetic materials designed to offer the benefits of both. Biosynthetic substitutes provide an optimal environment for wound healing by supporting cell attachment, growth, and tissue integration. Some examples include:
- Biobrane: A silicone-based biosynthetic skin substitute with a nylon mesh containing collagen, which provides both a protective barrier and promotes healing.
- Integra: Made of a silicone layer (acting as the epidermis) and a collagen-based matrix (acting as the dermis), it encourages cell migration and new tissue formation.
How Skin Substitutes Promote Wound Healing
The effectiveness of skin substitutes lies in their ability to replicate the skin’s protective and regenerative functions. Here’s how they revolutionize wound healing:
- Enhanced Healing Environment: Skin substitutes maintain an optimal moist environment for wounds, which is crucial for faster healing. This environment not only prevents dehydration of the wound bed but also accelerates the migration of cells necessary for tissue regeneration.
- Reduction of Infections: By providing a barrier against external contaminants, skin substitutes reduce the risk of wound infections. This is particularly beneficial for burns and chronic wounds that are prone to infection.
- Reduction in Healing Time: By stimulating the body's natural healing processes, skin substitutes can significantly reduce the time required for wound closure. This results in less scarring, improved skin function, and better overall outcomes for patients.
- Support for Chronic Wounds: For patients with chronic wounds, such as diabetic ulcers or venous leg ulcers, skin substitutes offer a vital solution when conventional treatments fail. They can promote tissue growth, reduce pain, and help close wounds that would otherwise remain open for extended periods.
- Lowering the Need for Skin Grafts: In cases of severe burns, the availability of healthy skin for grafting can be limited. Skin substitutes can either serve as a temporary covering to prepare the wound bed for future grafts or as a permanent solution, reducing the need for additional surgeries.
Clinical Applications of Skin Substitutes
Skin substitutes have found applications in a variety of clinical settings, including:
- Burn Care: In burn management, skin substitutes can serve as temporary covers to protect the wound, reduce fluid loss, and minimize pain. They also support the growth of new tissue, essential for healing extensive burn injuries.
- Chronic Wound Treatment: For conditions such as diabetic foot ulcers, pressure ulcers, and venous leg ulcers, skin substitutes provide a scaffold for cell migration and tissue regeneration, promoting faster wound closure.
- Surgical Wound Healing: Post-surgical wounds, especially those that do not heal properly, can benefit from skin substitutes by improving the healing environment and reducing the risk of complications.
Future of Skin Substitutes in Wound Care
Advancements in biotechnology continue to drive the development of more sophisticated skin substitutes. Researchers are working on creating more personalized, adaptable, and functional substitutes that closely mimic the properties of natural skin. Innovations in 3D bioprinting, stem cell technology, and tissue engineering hold promise for the next generation of skin substitutes, potentially leading to faster healing times, reduced scarring, and improved patient outcomes.
Conclusion
Skin substitutes are undoubtedly revolutionizing wound healing by offering effective alternatives to traditional methods. Their ability to create an optimal healing environment, reduce the risk of infection, and promote faster tissue regeneration makes them invaluable in treating complex wounds. As research and technology continue to advance, the potential for skin substitutes to further enhance wound care outcomes is immense.